New seminar series has global reach
Two academics at Southampton Solent University have launched a successful seminar series.
11 December 2025
Two academics at Southampton Solent University have launched a successful seminar series.
11 December 2025
Students from Southampton Solent University's School of Creative Industries have had a unique opportunity to showcase their skills.
5 December 2025
Will Swain, a BA (Hons) Television Production graduate has received a prestigious industry award.
1 December 2025
Solent Creatives, Southampton Solent University's student-powered creative agency, has collaborated with charity, Step by Step.
28 November 2025
A new series of masterclasses is inviting music students at Southampton Solent University to take the lead.
27 November 2025
Associate Professor, Dr Roy Hanney penned an opinion piece, published by HEPI.
26 November 2025
The budget today confirms a government focused on stability rather than sweeping reform says business expert.
26 November 2025
Students at Southampton Solent University successfully ran the livestream for the 2025 COPD Big Baton Pass.
21 November 2025
Dean of the School of Business, Law and Society, Professor Lois Farquharson dives into the power of storytelling in retail adverts.
20 November 2025
Southampton Solent University welcomed a delegation from India on Tuesday 18 November.
19 November 2025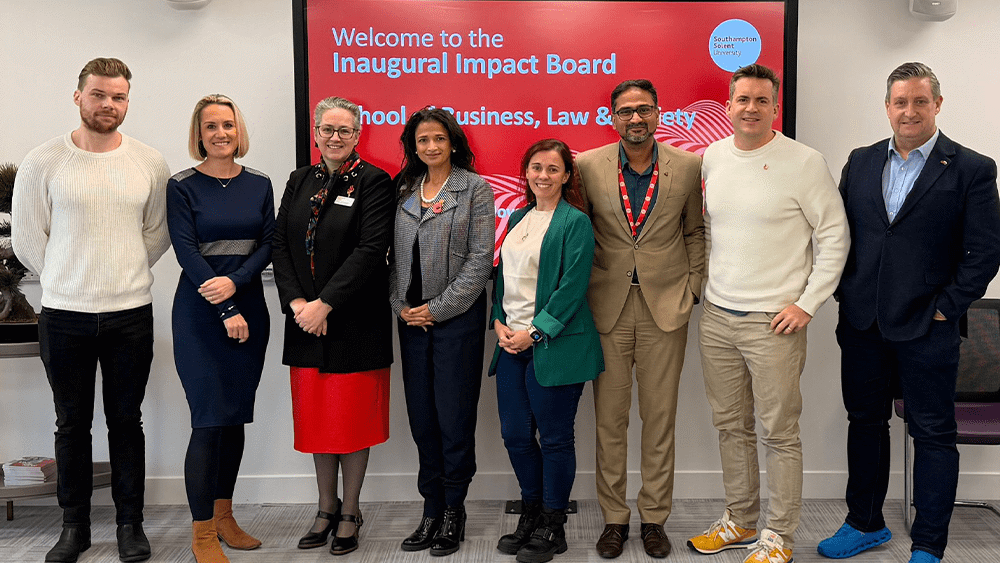
Southampton Solent University has held its inaugural meeting for the School of Business, Law and Society's new Impact Board.
17 November 2025
Experience life as a student at Solent at one of our on-campus or virtual undergraduate, postgraduate or maritime open days.
Find out more
Solent students supported the BBC's Children in Need fundraising efforts
6 November 2025
Solent welcomed civic and business representatives to discuss the university's role in the future of the region
5 November 2025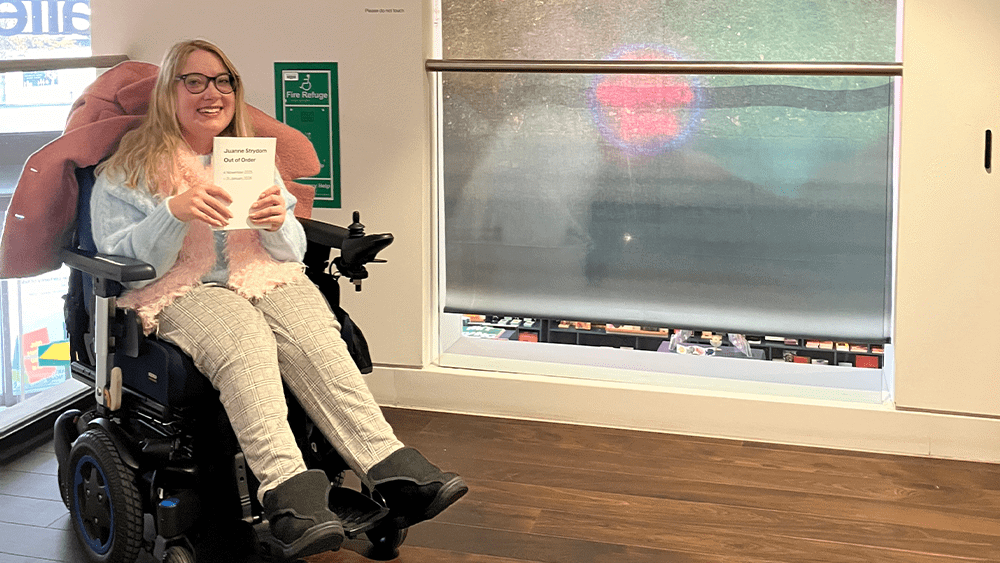
Southampton Solent University is celebrating PhD candidate, Juanrie Strydom, who has achieved her first solo exhibition.
5 November 2025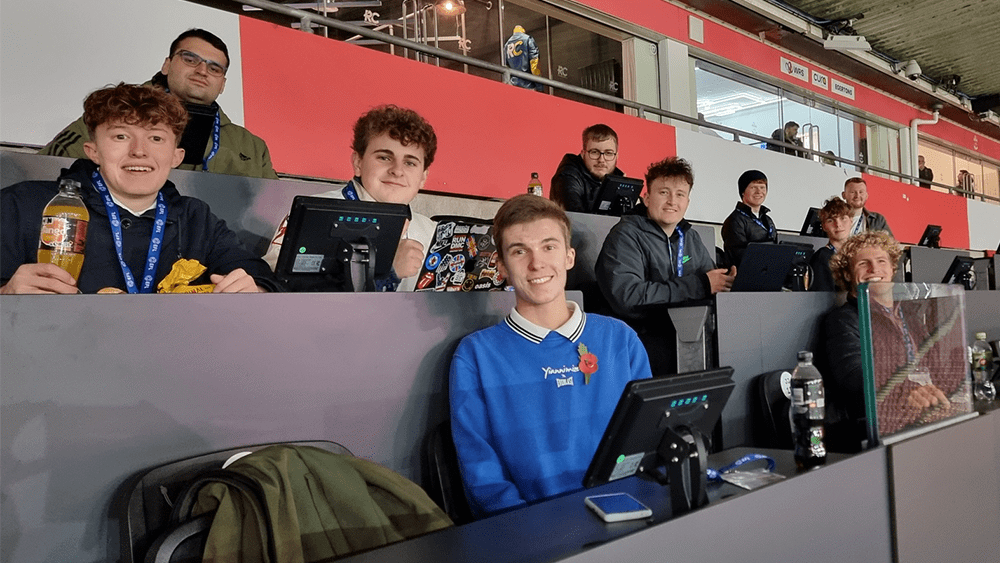
BA (Hons) Sports Journalism students recently visited St Mary's Stadium to report on an Under 21s game against Real Madrid.
31 October 2025